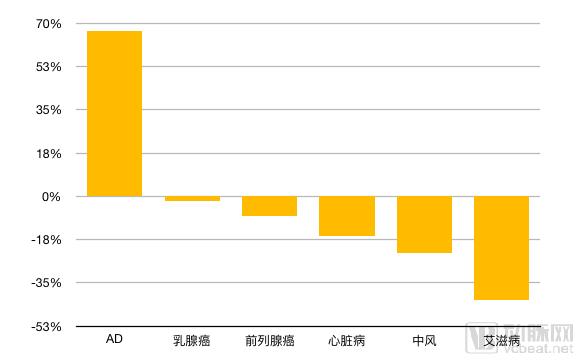
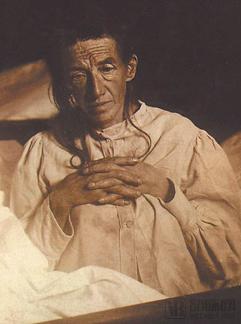
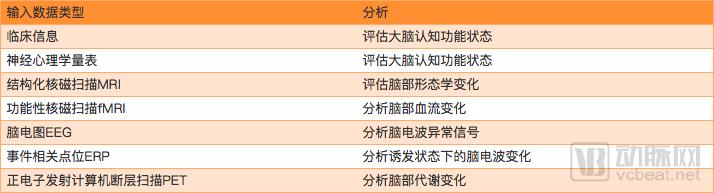
"We become ridiculous, incompetent and funny. But this is not what we are, it is our disease." In Alice, Alzheimer's early onset patient Alice said. Alzheimer's disease (abbreviated as AD) exists around us and is more common in the elderly after the age of 65. Like many chronic diseases, it seems to be fierce without cancer, but the damage done to patients and family members is hard to estimate. When we witnessed the love of our loved ones on the road to life, decades of wisdom gradually dissipated, and slowly left an old body, which may be more terrible than the pain of the physical. As of 2015, the total number of AD patients worldwide has reached 46.8 million, and the number of patients in China has exceeded 6 million. According to the same year, AD has a new symptom every 7 years. According to the first discovery of AD for more than 100 years, humans have not found a cure for AD, and even did not fully understand its pathology. This does not mean that human beings are inactive. In fact, many generations of scientists have been working for this century. Percentage change in mortality from 2000 to 2010 Three people, a century, Alzheimer came to us In June 1864, the German Alzheimer was born in Bavaria, and the excellent family gave him a good development environment. In order to give young Alzheimer the opportunity to participate in the Royal College of Humanities, the Alzheimer family moved from Bavaria to Berlin, and he himself successfully entered Würzburg to study medicine. In 1901, Alzheimer lost her wife Cecily, but the pain of losing her wife gave him the motivation to study. This year, he observed a 51-year-old female patient Augustus in his psychiatric hospital. (Auguste Deter), her strange symptoms such as short-term amnesia make everyone puzzling, Alzheimer is fascinated by her. An interview record that has been passed down to the present reflects the Augustus and is also the desperation of many elderly dementia patients. "Write a 5." "A woman." Augustus wrote. "Write an 8." "Augustus." She wrote her name. In the process of writing, she repeatedly mourned "I have lost myself, so to say..." Alzheimer's disease is not a transient process of amnesia. She knew that she was losing herself, but she could do nothing. Augustus In 1906, Augustus came to the end of his life and contributed her brain to scientific research. Alzheimer brought her case and brain to Munich to continue her research and found that her cerebral cortex deposited a special substance and many tissues in the cerebral cortex were already necrotic. Alzheimer used Bielschowsky's staining technique to discover two abnormalities in her brain: amyloid plaques and neurofibrillary tangles, which became the hallmarks of later judgments of Alzheimer's disease. But this result did not attract the attention of the medical community at the time. Until 1910, his boss and research partner Emil Kraepelinz in the "Handbook of Psychiatry" book, the official name of this strange disease Alzheimer's disease. In the following 70 years, AD research in the medical field continued, but the development of science and technology was limited, and there were not many outstanding achievements. By the 1970s, AD gradually entered people's lives. In 1974, the US Congress established the National Institute for Aging (NIA) under the National Institute of Health (NIH). In the same year, brain psychologists Davies and Maloney proposed the theory of cholinergic deficient, which is still the main principle of drug inhibition of AD deterioration. Here, one person is also involved in the research career of AD because of his wife. He is called Jerome H. Stone. The wife of this famous businessman was first diagnosed with AD in 1970, even though the family's wealthy face to such a terminal illness can not do anything. Stone was surprised at the fact that there was so little information about AD in the world. Since then, he has frequently communicated with many neurologists and tried to organize related scholars. In 1980, the Alzheimer's Association was established and Stone was the first president of the association. So far this association still has a major influence in the field of mental illness. Learn about today's Alzheimer's disease from a set of data According to 1998 statistics, AD is the third most expensive disease in the United States, second only to cancer and cardiovascular disease. On average, the daily cost per AD patient is three times that of a normal person. The AD drug market was $5.8 billion in 2011, and this number is expected to reach $14.5 billion in 2020. In 2014, long-term care costs for AD patients totaled $214 billion, and are expected to reach $1.2 trillion by 2050. According to data released by the International Association for Alzheimer's Association, in 2013, the number of people with dementia worldwide was 44 million, of which 50%-75% were AD patients. In 2015, there were 9.9 million new dementia patients worldwide, with an average of 1 additional every 3 seconds. Globally, the total cost of nursing Alzheimer's in 2015 is estimated at $818 billion, an increase of $214 billion compared to 2010. So, what factors are related to AD? Age is an important factor affecting AD. One study showed that AD patients under the age of 65 accounted for 4% of the total number of patients, 6% of patients aged 65-74 years, and 44% of patients aged 75- Between the ages of 84, the number of patients over the age of 85 accounted for 46%. At the same time, the probability of women being sick is about twice that of men. Second, genes are another important factor. It is known that there are three genes associated with early-onset AD, APP (amyloid precursor protein) on chromosome 21; PSEN1 (presenilin 1) on chromosome 14 and PSEN2 on chromosome 1 ( Presenilin 2) Late onset AD is associated with several SORL1 genes on CR1, PICALM, TREM2, and chromosome 11. In order to solve these problems, domestic and foreign companies have invested in AD-related treatment, and the arterial network has compiled some companies that have recently obtained financing. We can see some trends. Some AD corporate financing and business conditions (excluding large pharmaceutical companies) Predicting is the best way to deal with AD today. If clinical treatment can delay the patient's late onset for one year, then 9 million patients will be reduced. Every Alzheimer's disease in developed countries consumes an average of $33,000 a year. Early diagnosis and diagnostic interventions can significantly delay the patient's admission to the care facility, resulting in an average annual savings of $10,000. If you can postpone 5 years, you can solve $5 trillion in 30 years. In the past, AD detection was performed by using lumbar puncture to extract cerebrospinal fluid, and Aβ amyloid and Tau protein were detected. This type of hair requires pre-injection of anesthetic, which can cause severe neuropathic pain after wearing the waist, which is often difficult for patients to accept. Nowadays, the use of artificial intelligence to screen and diagnose AD is becoming more and more mature, and many companies have already put the corresponding products in the hospital. This technology not only eliminates the patient's invasive testing, but also produces quantitative results in a short period of time. Avalon AI from the UK predicts the risk of developing AD in the future through brain MRI images. They use deep learning technology to develop computer medical imaging diagnostic tools, and the current effective prediction accuracy for Alzheimer's has reached 75%. The domestic AI company Yasen Technology combines clinical medical records, neuropsychological scales, EEG and various image data to analyze the patient's brain conditions, using multimodal and deep learning techniques, and based on Chinese group standards. The brain template and the AD-specific disease database for five consecutive years of training, training diagnostic and predictive models, can classify patients with dementia disease and predict disease duration within five years, and generate a structured report. The highlight of Yasen’s AD diagnostic prediction system is that it assists the clinician in making the diagnosis, and the data can be evidence-based and traced; the patient is accurately classified, including normal aging degeneration, forgetful mild cognitive impairment (aMCI), Implementation of dysfunctional mild cognitive impairment (dMCI), Alzheimer's disease (AD) and other types, making treatment more effective; for patients without serious symptoms, early warning, early effective intervention. Accurate typing is also important for new drug development and testing, helping to identify differences in the characterization of different markers among different types of patients. Yasen Technology Multimodal Data Analysis Stage awareness is very effective in dealing with dementia diseases. Many domestic patients have entered the stage of performing dysfunctional mild cognitive impairment (dMCI) or AD during the examination, so early screening is very necessary. For dementia-type diseases, only early detection and corresponding intervention are given at this stage. In order to delay the arrival of AD. Another domestic company, Nuo Nuo Technology, is also predicting progress on AD. Ninuo artificial intelligence EEG analysis system can solve EEG reading problems and make EEG inspection a pre-primary screening for other testing items (such as images). The project can also be used in conjunction with blood testing and imaging projects for comparative validation studies. Ni Nuo Technology currently focuses on epilepsy and AD optimization related algorithms. In an interview with Arterial Network in July, its founder Dai Wei said that in the future, the company will expand to various types of EEG diseases. "EEG equipment can be applied to multiple departments. At present, we use epilepsy as the entry point. Because EEG needs for epilepsy are the most rigid, it is based on EEG diagnosis as a gold standard, and there are no other more effective diagnostic methods. Of course, we are not limited to epilepsy, but use this as a breakthrough to establish a pathology database. Once the database is established, any disease department that requires EEG detection, including AD, can be entered." Founded in 2017, 铱硙Medical Technology Co., Ltd. has also set its sights on the big market of AD. Its brain doctor intelligent diagnosis cloud platform system uses AI technology for early screening and diagnosis of AD. The hospital conducts clinical trials with an accuracy rate of 85%. By collecting brain MRI data from a large number of Chinese people, the Brain Doctor System builds a brain imaging database of the Chinese population to accurately detect and evaluate brain morphological data of each subject. Through cooperation with many top hospitals in China, tens of thousands of high quality standard medical image data have been obtained. Can we cure AD? The first treatment to introduce AD ​​is not medication, but a method called nostalgic therapy that treats patients by psychological suggestion. Hsieh and other scholars conducted a 12-week randomized controlled trial in 61 patients with mild to moderate dementia in the Taiwan Nursing Home. The psychiatric nursing staff developed a structured intervention program, which was administered once a week to the intervention group. Group nostalgic therapy in the form of a life review of 40 to 50 minutes each time encourages participants to tell their stories with old photos, records and other meaningful materials. The results showed that after the intervention, the Geriatric Depression Scale and the Apathy Symptom Rating Scale were used to measure the results. The results showed that the intervention group had significant improvement in depression, behavioral apathy and cognitive apathy, and the neuropsychology depression score was also significantly reduced. Therefore, group nostalgic therapy can effectively treat the apathy and depression of patients with mild to moderate Alzheimer's disease. Recently, the American company Smart Brain Aging launched a virtual online product similar to nostalgic therapy. Its Brain U Online platform can provide users with more than 20,000 various cognitive skills related exercises online, with content processing speed, Memory and attention are at the core. Hundreds of similar exercises can be redesigned for use on the mobile Internet through the app. At the same time, the program also includes a virtual classroom that allows users to participate in social activities and engage in conversations with others. Through data provided by the company, the product can reduce the negative cognitive impact of Alzheimer's disease by 45% and delay its progress by 2.5 years. Although nostalgic therapy can interfere with mild to moderate AD, it is still weak for patients who have already shown severe AD symptoms. In 1978, NIA teamed up with Warner-Lambert Pharmaceutical Company (now Pfizer) to begin a clinical trial of the first drug to treat AD symptoms. Until 1993, the FDA officially approved the first drug for the treatment of AD, Tacrine. An important cause of AD is acetylcholine deficiency, which leads to memory loss, loss of orientation, behavior and personality changes, while tacrine can inhibit cholinesterase, promote the release of acetylcholine in the brain, and increase its content. The disadvantage of this drug is that the half-life is extremely short and requires daily medication, which has a greater damage to the liver. In the next decade, as a representative of the improvement of choline neurotransmitter drugs, Arisin, Assin, and Galantamine also passed the FDA. The researchers also tried to develop a number of drugs through other channels, including improving brain blood circulation and brain cell metabolism; using calcium antagonists to reduce nerve cell damage or death caused by calcium influx; using hormone drugs to relieve symptoms of patients. In 2015, the team of Professor Yurgen Goetz of the University of Queensland discovered a new approach that is expected to be used to treat AD. His and colleagues' research shows that the ultrasound treatment of repeated scans of AD mice can effectively open the "blood-brain barrier" of the small book without causing ischemic injury and neuronal degeneration, allowing the drug to enter the mouse brain. In turn, the Aβ protein is effectively cleared, and the memory function is also repaired. In recent years, many large pharmaceutical companies have launched corresponding new drug research and development projects for the cure of AD. However, due to the slow progress of AD and the high cost of research, some companies have to announce the abandonment of the corresponding research. Among them, one of the lessons of experimental failure is that patients did not have a brain scan before entering the trial. Many patients did not respond to the drug without distinguishing the different types of dementia, even without diagnosis. In January 2018, Pfizer announced the closure of its AD and Parkinson's disease drug development, Roche's new drug also failed in the clinical stage, and other companies are similar. So, so far, we still can't talk about "cure", we can only hope to find out early to delay the onset of the disease. Latest research progress On June 24, 2018, a study published in the journal Neuron, a journal of Cell Publishing, used the big data method to reveal an incredible potential cause of the disease - viral infection. Beta amyloid, the main direction of the past few decades, may not have much to do with the treatment of AD. In this study, scientists first analyzed 944 brain samples, of which 622 were from AD patients and 322 were from healthy donors. They did two tests, the first one is to analyze the DNA, to understand the difference between the genetic information of the two; the second is to analyze the RNA to see if the gene expression levels of the two are consistent. The results showed that the gene expression patterns of patients and healthy people were significantly different. In the brain samples of patients, they found that the levels of two types of human herpesviruses increased significantly and were positively correlated with the symptoms of AD. Scientists have found that they can affect the expression of "classic" AD genes such as BACE1, PSEN1, and APBB2 in brain cells. In other words, many of the symptoms we see may be the result of a viral infection. Based on the above results, the researchers can not assert that AD is caused by viral infection, and the results of the study need to continue to demonstrate. Written in the future Even if it may cost $1 billion for a phase III clinical trial, even if it has been 15 years since the last AD drug was launched, we may have to wait for the next 15 years, and there are still many giant companies continuing to move forward in this field. With the improvement of people's awareness of AD and prevention of disease, more and more people believe that AD patients can not start treatment after they have been diagnosed. At this stage, early predictive prevention is the best way to improve the quality of life. Some pharmaceutical companies have begun drug testing in people who are susceptible to AD but have not yet developed symptoms. Therefore, we can expect to establish a link between "the past self" and "the future self" and grasp it in the hands of human beings. Attachment: AD related timeline On November 3, 1906, the first AD was confirmed by Alois Alzheimer. In 1910, psychiatrist EmIll Kraepelin coined the name "Alzheimer" in a 1910 medical book. In 1932, Schottky first reported cases of autosomal dominant AD. In 1940, Van Bogaert, 1946 Essen-Moller reported familial AD pathology. In 1963, electron microscopy revealed that the double helix filamentous material formed a neurofibrillary tangles. In 1974, the National Congress established the National Institute for Aging (NIA) as part of the NIH Institute. 1976, Dr. Robert Katzman claims that AD is the most common form of dementia and a major public health challenge. This sparked attention to AD and launched many brain-related projects through the NIH. In 1978, NIA teamed up with Warner-Lambert Pharmaceutical Company (now Pfizer) to begin a first clinical trial of a drug designed to treat the symptoms of AD. In 1979, Jerome Stone and other members of the AD family met with the NIA this year. In 1980, the Alzheimer Association was established. From the meeting in 1979. Stone served as the first president. In 1984, beta-amyloid was discovered as the main substance of AD. In 1986, tau protein was discovered and confirmed as the main substance of AD. In 1986, nostalgic therapy was introduced into the care of Alzheimer's disease by Norris. In 1990, St George-Hyslop discovered the genetic heterogeneity of AD. In 1991, Goate et al found a missense variation in the APP gene in a family genetic disease case. In 1993, the FDA officially approved the first cholinesterase inhibitor Tacrine (Tacrine). Four AD drugs were approved in the next decade. In 1994, on November 5, former US President Ronald Reagan was diagnosed with Alzheimer's disease. In 1995, Games et al. established an APP transgenic mouse model. In 1999, Vassar et al. located a cloned beta secretase. Schenk and other leading active immunotherapy have been successful in animal vision. Petersen et al. proposed the concept of “mild cognitive impairmentâ€. In 2003, genetics research began, and the Alzheimer Association and NIAk began accepting people to participate in the National Alzheimer's Disease Genetic Study, which was funded by the federal government. In 2017, AI technology was used to test AD, and Yasen Technology, Brain Doctor and other companies developed related products. In January 2018, Australian and Japanese scientists developed a blood test that detected proteins associated with Alzheimer's blood. On June 23, 2018, it was newly discovered that viral infections may cause AD.
The foot and ankle locking plate is a special-shaped plate specially developed for calcaneal and ankle fractures, which is in line with the anatomical structure of the calcaneal and ankle joints.
During the postoperative treatment process, it can reduce the stimulation of surrounding tissues and promote bone healing.
The calcaneus is the largest of the seven tarsal bones and is located on the lower back of the foot, forming the heel. Calcaneal fractures are relatively rare, accounting for 1% to 2% of all fractures, but are important because they can lead to long-term disability. The most common mechanism of severe calcaneal fractures is axial loading of the foot after a fall from height. Calcaneal fractures can be classified into extra-articular and intra-articular fractures. Extra-articular fractures are generally easier to assess and treat. Patients with calcaneal fractures often have multiple comorbid injuries, and it is important to consider this possibility when evaluating patients.
The ankle joint is composed of the articular surface of the tibia, the lower end of the fibula, and the talar trochlea, so it is also called the talar calf joint. Ankle fractures, including fractures of the medial malleolus, lateral malleolus, posterior malleolus, or fractures of varying degrees occurring simultaneously, are due to greater violence to the medial and lateral malleolus. At the same time of both ankle fractures, the talus directly impinges posteriorly or impinges on the tibia when displaced by external rotation. Fracture of the posterior malleolus due to the posterior margin.
Foot Mini Locking Plate is composed of 2.7mm series of mini locking plate, covering a variety of plate types, widely used in trauma fixation and orthopedic surgery of the forefoot. Anatomical design of bone plate to reduce the need for shaping.
orthopeadic implant,calcaneal stress fracture,calcaneus bone,calcaneus fracture Jiangsu Aomed Ortho Medical Technology Co.,Ltd , https://www.aomedortho.com